The healthcare industry is currently grappling with what has been termed the “Big Squeeze,” a combination of rising costs, shrinking margins, and increasing demands for higher quality care. These pressures are particularly acute for healthcare organizations that provide Durable Medical Equipment (DME) and Home Medical Equipment (HME). Yet, by adopting innovative strategies and leveraging advanced technologies aimed at reducing healthcare costs, these organizations can not only survive but thrive in this challenging landscape.
The Economic Landscape: Understanding the Big Squeeze
Several factors are driving the Big Squeeze in healthcare. The aging population, particularly the baby boomers, is significantly increasing the demand for healthcare services. By 2030, all baby boomers will be over the age of 65, leading to higher rates of chronic diseases and increased healthcare utilization. The U.S. healthcare expenditure is projected to reach $6.2 trillion by 2028, with the costs associated with aging and chronic diseases being major contributors (CMS).
Compounding these demographic pressures are ongoing staffing shortages. According to the Association of American Medical Colleges, the U.S. could see a shortage of up to 124,000 physicians by 2034.
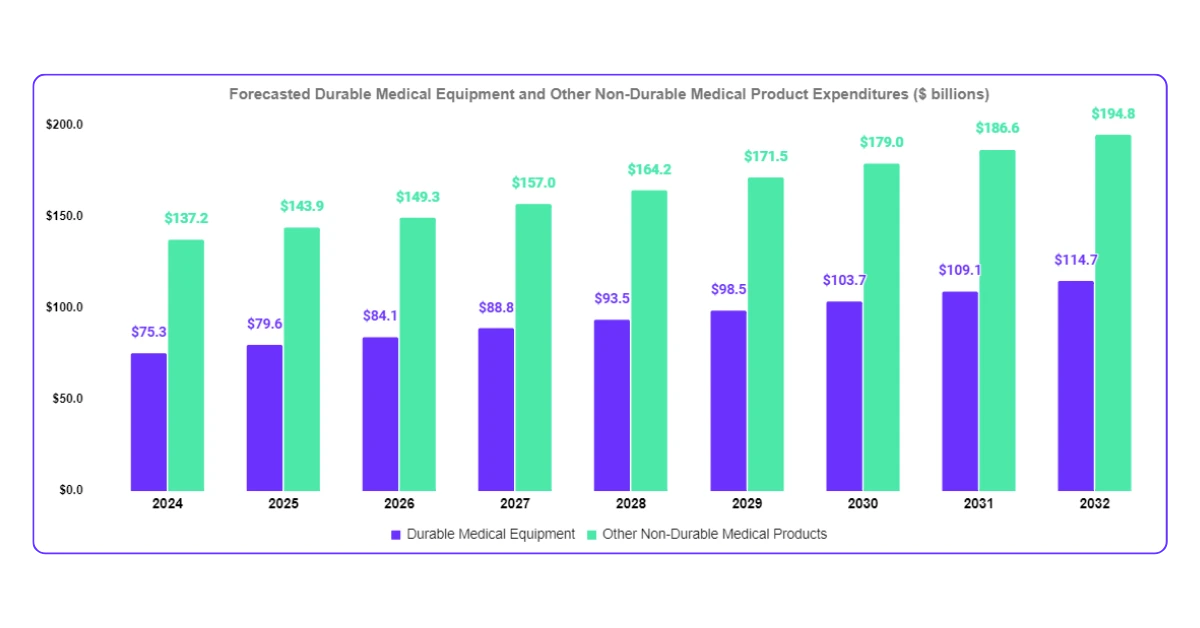
Adding to the strain is the growing cost of Durable Medical Equipment (DME). Expenditures on DME are projected to increase by 46.26% by 2030, reaching $32.8 billion (CMS).
These converging factors are creating a perfect storm that is squeezing healthcare providers, payers, and patients alike.
The Role of DME in the Healthcare Ecosystem
DME plays a crucial role in patient care, especially as more services shift from hospitals to home settings. The global DME market is expected to grow at a compound annual growth rate (CAGR) of 5.6%, reaching $93 billion by 2030 (Grand View Research). Despite its importance, the DME management process remains fragmented and inefficient. Nurses, who are often responsible for coordinating DME, must navigate complex systems, leading to delays, errors, and increased costs.
These inefficiencies are a major contributor to the staggering $265.6 billion wasted annually in healthcare due to administrative complexity alone, a significant portion of which could be mitigated through more efficient DME management (JAMA). In fact, up to 30% of overall healthcare spending is considered wasteful, with inefficiencies in care delivery and administrative burdens being primary contributors (JAMA).
Strategies for Thriving Amid Economic Pressures
To thrive in this environment, healthcare organizations must adopt strategies that streamline operations, reduce costs, and improve patient outcomes. Here are several key approaches:
-
Optimize DME Management with Integrated Systems:
Integrated DME management systems significantly reduce administrative burdens and improve efficiency. These systems offer a centralized platform where clinicians can order and track equipment, automate workflows, and ensure timely delivery. By eliminating manual processes and reducing the potential for errors, these systems help healthcare providers focus more on patient care and less on logistical challenges.
-
Leverage Data for Better Decision-Making:
Data-driven decision-making is essential in navigating the Big Squeeze. Advanced DME systems provide real-time insights into inventory levels, patient needs, and equipment utilization. By harnessing this data, healthcare organizations optimize their DME processes, reduce unnecessary inventory purchases, and ensure that the right equipment is available when needed. According to a study by McKinsey, leveraging data analytics in healthcare could save the industry up to $450 billion annually by optimizing efficiency and reducing waste.
-
Embrace Value-Based Care with DME as a Catalyst:
The shift towards value-based care demands a focus on outcomes, not just volume. DME plays a critical role in preventing costly hospital readmissions. By ensuring patients have the necessary equipment at home, providers improve patient satisfaction and reduce overall healthcare expenditures. Approximately 76% of hospital readmissions are preventable, representing a potential $17 billion in savings for Medicare alone (PLOS ONE).
-
Empower Your Staff for Success:
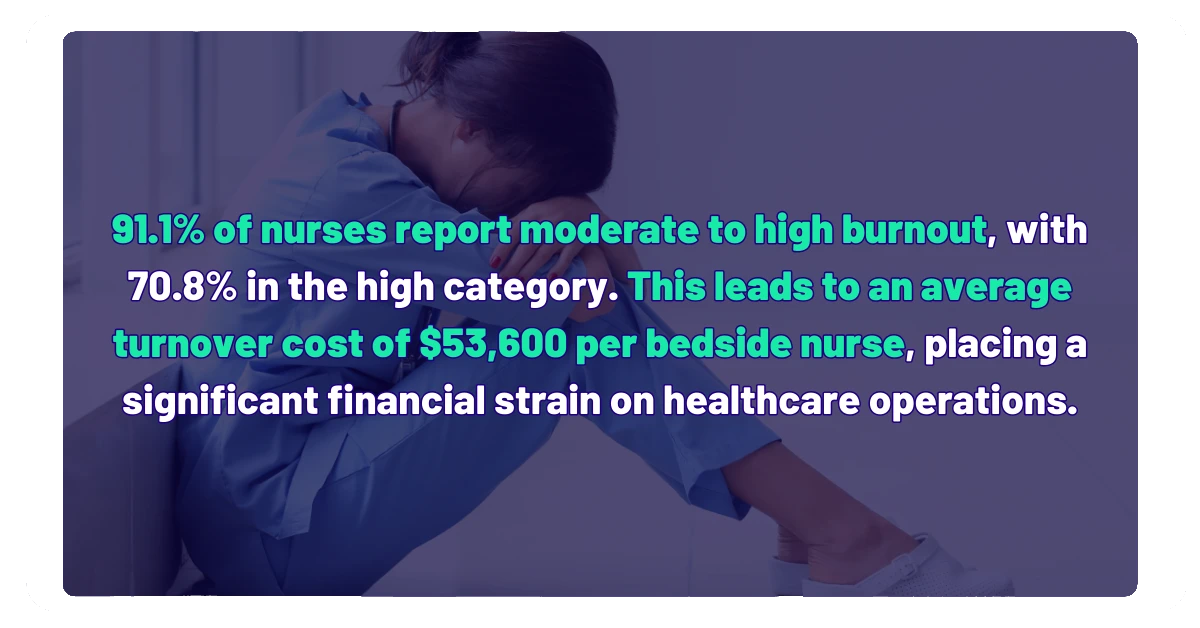
As healthcare organizations implement new technologies and processes, it is vital to invest in staff training and support. Nurses and other frontline staff need to be equipped with the skills and knowledge to effectively use integrated DME systems. This not only improves efficiency but also enhances job satisfaction, which is crucial in an industry plagued by burnout and staffing shortages. According to a recent study published on the National Library of Medicine, it was found that 91.1% of nurses report moderate to high levels of burnout, with 70.8% in the high category. This burnout has serious financial implications, as hospitals face an average turnover cost of $53,600 per bedside nurse due to burnout-related turnover, further straining healthcare operations (ANA).
Conclusion: The Healthcare Industry Is at a Crossroads
Economic pressures, staffing shortages, and increasing patient demands are converging to create a perfect storm. However, within these challenges lies an opportunity for transformation.
By adopting innovative solutions, leveraging data, and focusing on value-based care, healthcare providers can navigate the Big Squeeze and emerge stronger. Integrated DME management systems offer a path forward by reducing inefficiencies, improving patient outcomes, and ultimately driving long-term profitability.
As the healthcare landscape continues to evolve, organizations that embrace these strategies will be well-positioned to thrive in the face of ongoing challenges. Now is the time for healthcare leaders to take proactive steps, ensuring that their organizations are prepared to meet the demands of the future.
Ready to future-proof your healthcare organization? Contact us today to learn how we can help you optimize your operations and stay ahead in an ever-changing industry.




